Mastering Supportive Stance CPI: A Practical Guide to Preventing Restraint
Supportive Stance Crisis Prevention Intervention (CPI) (a non-violent crisis intervention technique) transforms how we approach individuals in crisis. It's a shift from forceful control to understanding and connection, significantly reducing the need for physical restraints. This approach prioritizes building bridges of trust and de-escalating situations before they escalate, creating a safer environment for both patients and staff. How can we effectively adapt our techniques to prevent restraint and ensure a safer and more supportive environment?
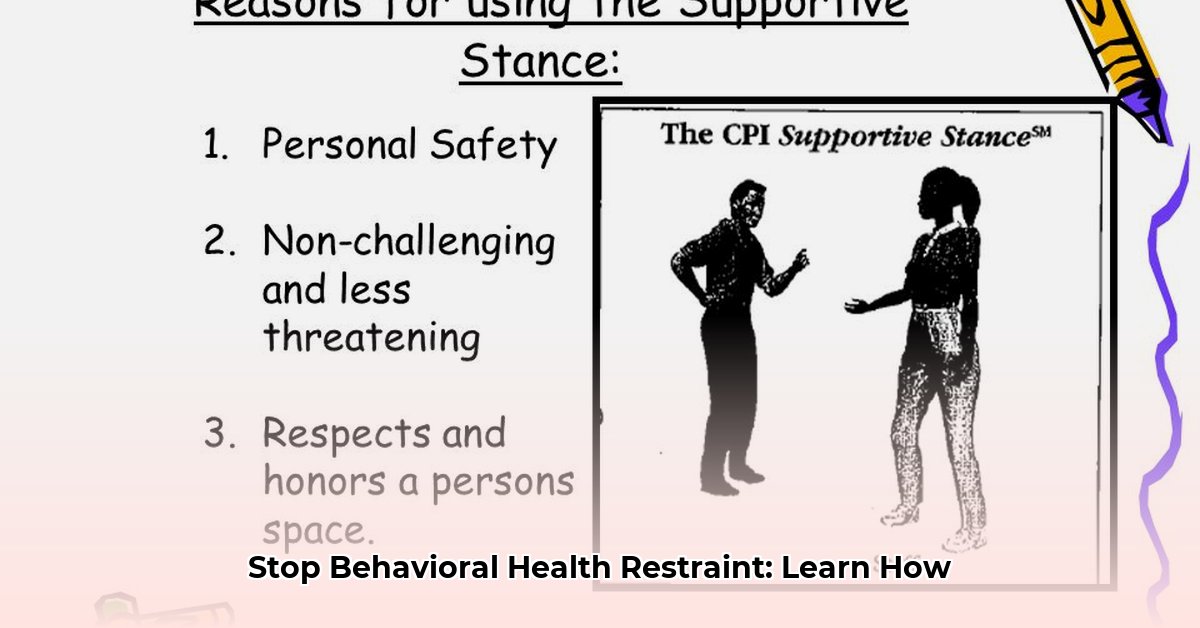
Understanding the Supportive Stance: More Than Just a Technique
The Supportive Stance emphasizes empathy and respect. We approach individuals with understanding, acknowledging their feelings even if we don't condone their behavior. It involves actively listening and validating their experience. Think of it as calming a frightened person, providing support rather than escalating the situation through defensive reactions.
Implementing Supportive Stance CPI: A Step-by-Step Approach
This section provides a step-by-step guide to implementing the Supportive Stance CPI technique. Each step is crucial to de-escalating a situation safely and effectively.
Step 1: Rapid Situation Assessment: Quickly observe the individual's behavior, emotional state, and environment. What triggers their distress? Are they communicating effectively? This assessment informs your approach. What specific behavioral cues might signal an imminent escalation?
Step 2: Safe Proximity and Nonverbal Communication: Approach close enough for effective communication but maintain safety. Use open posture (avoid crossed arms or defensive stances). Subtly mirroring their body language (e.g., mirroring their slight forward lean) can build rapport. How can maintaining an open posture increase trust and reduce defensiveness?
Step 3: Verbal De-escalation: The Power of Calm Communication: Speak calmly, clearly, and concisely. Active listening is crucial. Reflect their feelings ("You seem very upset"). Validate their experience, acknowledging their emotions without condoning the behavior. Use open-ended questions instead of demanding yes/no answers. What are the crucial elements of effective verbal de-escalation?
Step 4: Guiding, Not Controlling: The goal is to help the individual regain control, not to forcefully control them. It's a balance of support and limit-setting.
Step 5: Setting Clear, Respectful Boundaries: Communicate safety expectations and guidelines calmly and respectfully. Maintain professional boundaries while showing empathy. How can clear boundaries be established while still maintaining empathy?
Step 6: Offering Choices: Empowerment Through Agency: When safe, offer limited choices to empower the individual and give them a sense of control (e.g., "Would you prefer to sit down or stand?").
Step 7: Thorough Documentation: A Record for Safety and Learning: Detailed documentation is crucial for both patient safety and learning. Record observations, interventions, and outcomes. This information improves crisis response. What key information should be included in your documentation?
Real-World Example: Navigating an Anxiety Episode
Consider a patient experiencing a severe anxiety attack with agitated behavior. A Supportive Stance CPI approach would involve calmly approaching, using a reassuring tone and validating their feelings. Options might be offered: "You seem overwhelmed. Would you like to sit down, or perhaps some water?" This shift from control to collaboration de-escalates the situation, often eliminating the need for restraint.
Long-Term Strategies: Building a Culture of De-escalation
Supportive Stance CPI is an ongoing commitment, not a one-time training. Regular refresher courses, team debriefs, and a supportive workplace culture are essential. Investing in staff well-being is crucial because well-supported staff are less likely to encounter burnout, which can increase the likelihood of escalated situations.
Challenges and Solutions
Implementing Supportive Stance CPI faces challenges:
| Challenge | Mitigation Strategy |
|---|---|
| Staff Resistance to New Methods | Thorough training emphasizing long-term benefits (reduced restraints, safer environment, reduced stress) and ongoing support. |
| Limited Resources | Advocate for increased funding for training and support. |
| Ongoing Support Gaps | Establish mentoring programs, regular supervision, and opportunities for team debriefs. |
| Patient Unresponsiveness | Collaborate with other healthcare professionals to develop comprehensive, individualized plans. |
Mastering Supportive Stance CPI requires dedication, consistent practice, and ongoing learning. It's an investment in patient safety, staff well-being, and a therapeutic environment where everyone feels safe. It fosters better care, one interaction at a time.